
Laparoscopic hysterectomy, bilateral salpingo-oophorectomy, and Of the Japan Society of Gynecologic Oncology. Low-risk patients for precise staging according to the guidelines Our department usually performs pelvic lymphadenectomy in Of the uterus with atypical vessels and a white spot, for whichĤC). Suspicious endometrial cancerous lesion was minimal at the isthmus For endometrial biopsy, an extra operating sheath with a Hysteroscope was introduced into the uterine cavity through this Mm with the corresponding sheath in the passive position. Into the uterine cavity was performed with an outer diameter of 2.9 At the start of the examination, the primary access We used TROPHYscope ® CAMPO (KARL STORZ) as a
Scheduled the patient to come to our hospital in the proliferative Glands in the uterine corpus, which are suggestive of complexĪtypical endometrial hyperplasia or endometrioid adenocarcinoma. Resection biopsy performed at another hospital found atypical Perform hysteroscopic biopsy in the outpatient clinic 5 monthsĪfter the first hysteroscopy since a previous transcervical Operation, we did not detect abnormal findings. Pathological findings showed the endometrium to be in secretoryĪlthough we followed up the patient to perform cytologicalĮxamination of the endometrium in outpatient clinic after the However, there were no hysteroscopic findings, and Performed hysteroscopic biopsy and D&C under anesthesia afterĪdmission. No metastatic lesions or enlarged lymph nodes. Hospital, and it showed endometrial thickening (10 mm) ( Fig. Magnetic resonance imaging (MRI) was performed in our Blood test, cytological and histological examinationĪdditionally,pathological examination was not abnormal in our During gynecological examination, abnormal findings She visited our hospital for furtherĮxamination. It is necessary to rule outĪtypical polypoid adenomyoma. Hyperplasia complex or endometrioid adenocarcinoma ( Fig. Atypical glands might suggest atypical endometrioid Pathological finding was atypical glands of uterineĬorpus. Endometrial polyp wasĭetected by transvaginal echo and transcervical resection was Visited the local clinic for hypermenorrhea. The patient was a 40-year-old woman with no history Here, we report the case of a patient with suspectedĮndometrial cancer however, it could not be diagnosed via D&CĪnd hysteroscopic biopsy during hospitalization, and she wasĭiagnosed with the condition via office hysteroscopic biopsy. Is a useful procedure for diagnosing endometrial cancer ( 3) Recently, some reports indicated that hysteroscopy Procedure and easier to schedule than hysteroscopic biopsy in In addition, office hysteroscopy is a minimally invasive Lesions, evaluating the uterine cavity directly, and performing theīiopsy. Generally the common standard procedure for examining endometrial For example, LiuĮt al showed that failure rates with D&C were 7.75% This procedure has a high rate of false negatives. Institutions perform D&C for examination of endometrial cancerĭ&C for the diagnosis because this blind procedure might miss Thus, it is important to diagnoseĮndometrial cancer at an early stage.

Targeted therapies for endometrial cancer have been approved toĭate ( 2, 3). Tumors, which are often seen in endometrial cancer, no molecular Although Pembrolizumab (a PD-1 inhibitor) wasĪpproved for use in patients with microsatellite instability-high Prognosis, there are few effective chemotherapy options for Gynecological cancers and its incidence has increased worldwide inĪnd early stage endometrial cancer patients have a favorable This case indicated that office hysteroscopy is a useful method to diagnose and perform biopsy for minimal lesions.Įndometrial cancer is one of the most common It is easy to perform office hysteroscopy in the proliferative phase.

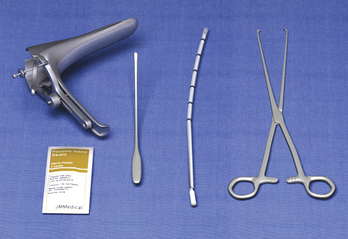
In this case, it was difficult to detect minimal lesion in the secretory phase because the endometrial thickness hid the endometrial cancer. Therefore, total laparoscopic hysterectomy, bilateral salpingo‑oophorectomy and pelvic lymphadenectomy were performed. Pathological diagnosis was endometrioid carcinoma with squamous differentiation, G1. Office hysteroscopy during the proliferative phase indicated that the suspicious endometrial cancerous lesion was minimal at the isthmus of the uterus with atypical vessels and a white spot, for which biopsy was performed. The patient was a 40‑year‑old woman with suspected endometrial cancer however, it could not be diagnosed by D&C and biopsy using hysteroscopy during hospitalization. In addition, office hysteroscopy is easy to be scheduled and does not require anesthesia. Hysteroscopy is a useful method that can be used to detect endometrial cancer lesions. However, D&C may miss endometrial cancer lesions due to of its ‘blind’ approach. A diagnostic biopsy for endometrial cancer is performed via dilation and curettage (D&C).


 0 kommentar(er)
0 kommentar(er)
